It was during this time that I had the opportunity to meet Doctor Don Berwick from the Institute for Health care improvement. Although we had attempted to improve our systems of care and had made some progress, I realized that there was much more that needed to be done in order to achieve improved patient safety.
At that time, we learned that it was not people that we should focus on, but it is systems. I learned quickly how the best individuals could make a mistake that might result in serious harm to a patient. We borrowed from other industries adopting simplification and standardization as a foundation for how we might address the human condition. By the human condition I mean that humans make mistakes and when we don’t have properly designed systems it is more likely that they will make a mistake. The way we can improve systems is to reduce their complexity, eliminate steps, and ensure that we are developing a standardized approach which helps deliver evidence-based care.
What outcomes?
Over many collaboratives around the world, we continue to support the development of capability of individuals to lead improvement by focusing on improvement tools, methods and measurement. It now has been over 20 years, and we still struggle to ensure that we’re providing safe care to our patients. We have focused on reporting systems to help us understand where the defects are in our system. We are focused on measurement in order to determine the performance of our systems. However even with all the work that we have undertaken we still are not as safe as other high-risk industries. I agree that there have been some improvements in some areas such as reduction of some central line infections, reduction of pressure injury, and reduction of catheter associated urinary tract infections. But could we not reach even higher levels of safety? There are many reasons such as organizations that feel that they’ve done all the work that needs to be done, leaders who no longer focus on safety as one of their top three areas, ever increasing complexity in the care that we deliver, patients who are older than require more complicated treatments, staffing shortages, and burnout.
Although it can be said that all of these are contributing factors, there is more that needs to be done. I continue to support standardization and simplification for those things that can be standardized. I also believe that we should continue to train people to learn how to improve rather than expect improvement without adopting a system that has the rigor and support such as the Model for improvement or Lean or any other improvement methodology that people are using. Each has its own advantages and disadvantages. I believe that must remind leaders at all levels of an organization to prioritize patient and staff safety. When we prioritize efficiency without considering its impact on safety, we put our patience at risk. As we’ve added more and more tasks to our doctors, nurses and other health professionals, we find that they must decide as to what they’re going to work on. As a result, oftentimes these individuals are forced to take shortcuts just to meet the demands of everyday care. The role that leaders can play and keeping patient and staff safety front and center will ensure that at the very least we will not lose any of the improvements that we’ve made.
During the past 15 years there’s been lots of discussion around the role of culture. Culture is something that’s difficult to grasp yet it is such an important influence on everything we do. Culture is a product of the behaviors that support our values. Each one of us is accountable for our behaviors. Leaders must provide clarity on which behaviors are expected and which will not be tolerated.
This realization of the role of culture is something that has been brewing in health care for some time and yet because we didn’t quite understand its role in improving patient safety, we did not focus on how to develop that enabling environment that a culture of safety provides. Over these many years I have been faculty for the Institute for Healthcare Improvement’s patient safety officer program. Working with an expert faculty with experience from all over the world, having participated in visits to numerous hospitals both those that are performing well and those that are not, and information from the many participants of the program, our faculty identified the key elements that are necessary in order to create that environment that allows us to reach higher levels of safety. The findings are represented in a graphic titled the Framework for Safe, Reliable, and Effective Care1 (Figure 1). That framework has three domains, one which focuses on the role of leaders, one which focuses on culture, and one which focuses on the learning system.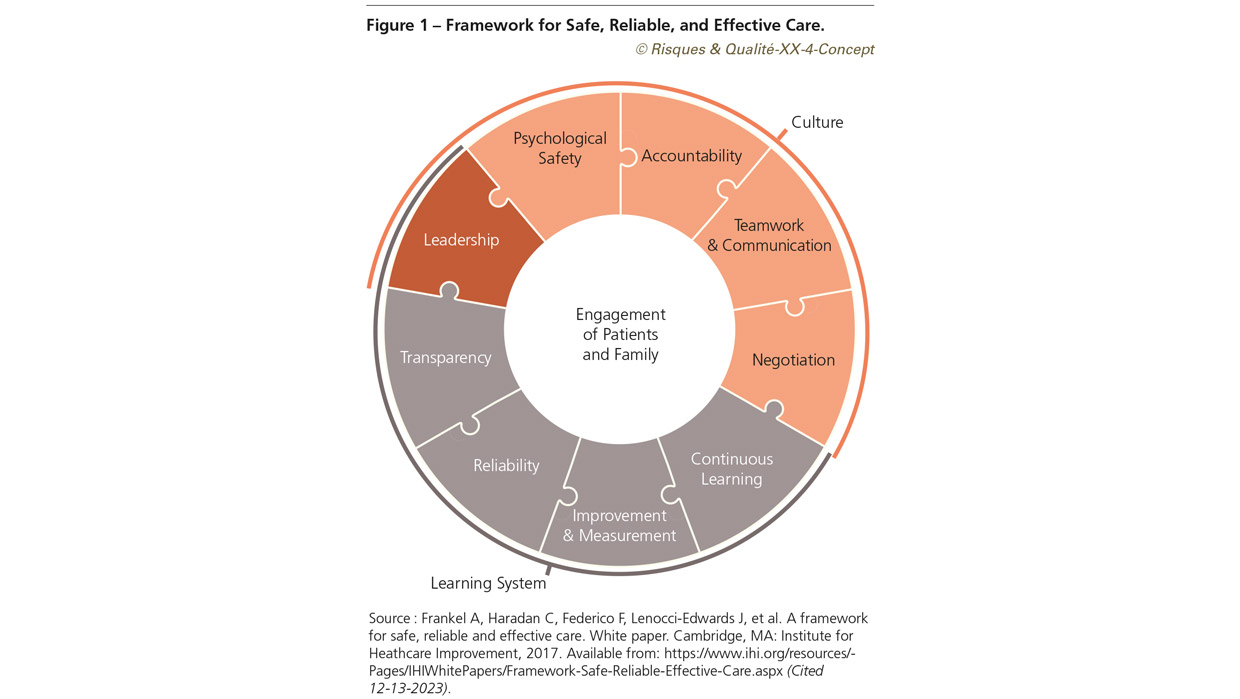
A framework to guide leaders
The role of leaders in an organization is not to be able to answer all questions but to guide individuals and provide them with the support that’s necessary to make improvement. It is also the role of leaders to ensure that there’s a learning system in which there is learning from what goes well and learning with what does not go well. We spend a lot of time looking for defects and then building systems to address those with the effects but not enough time in learning what really works in our existing systems. It is the behaviors of leaders that helps guide the rest of the organization and influence the development of that enabling culture. It starts with leaders who must hold themselves and each other accountable to ensure that desired behaviors are rewarded and supported and undesired behaviors are eliminated.
The next domain focuses on culture and includes elements such as psychological safety, a just and fair approach and accountability, teamwork and communication, and negotiation and alignment. As we speak of psychological safety we must focus on staff and patients feeling safe to ask questions when they’re not sure, to stop the line when they feel that the patient is at risk for harm, and to be able to admit that they may not know in front of others. The second element focuses on a just and fair approach when something goes wrong. Is often referred to as a just culture. We call it a just culture which is part of a culture of safety. It is how an organization responds when something goes wrong that greatly influences the formation and development of a psychologically safe environment. The approach begins not with the use of an algorithm but instead focuses first on determining if the defect is the result of a system issue. This change in approach sends a signal to staff that the organization is committed to not holding people accountable for system issues but holding individuals accountable for their behaviors. This does not mean that organizations should abandon the algorithms. It changes the sequence of the investigation, so it does not start with focusing on people.
The next element focuses on teamwork and communication. Our health systems are complex and require many individuals in order to deliver the care that a patient may need whether it be in a hospital or outside of the hospital. Often, we believe that we’ve communicated without fully appreciating whether our message was clear, understandable, and delivered in a way that allows the other person to question if something is unclear. A lot of time is spent on communication through various means. Yet few consider the difference between the intent of the message and the impact that it has on staff. Sometimes a well-intentioned message can be interpreted in a way that creates an unsafe environment or fosters lack of trust in those who delivered the message. Communication can be impacted by many things including use of jargon, terms that are unfamiliar to others, hearing disabilities, incomplete messages or messages that never reached the intended audience. I often hear that much of the communication happens via e-mail. Although this is one way of communicating, it is not always the best way, may not always be seen and read by everyone, and the tone can often be misinterpreted. Healthcare has adopted tools from other industries in order to facilitate communication amongst healthcare professionals. A common tool is referred to as SBAR which stands for situation, background, assessment, and recommendation.
Because sometimes there are conflicting opinions, effective teams must be able to resolve those conflicts and proceed to a solution that’s in the best interest of the patient. This element of the culture domain that deals with this is named negotiation or alignment. There are different ways in which individuals can negotiate in order to resolve a conflict. In a culture of patient safety, those conflicts are always resolved in the best interest of the patient and staff.
Conclusions
In summary, the culture that exists in an organization is the culture that may have suited the organization at some time. Today, we need a culture that supports and enabling environment where staff and patients feel safe in speaking up, individuals are not held accountable for system issues but are accountable for their behaviors, teams that communicate well among members, with other teams and with patients, and can reflect and solving problems in the best interest of the patient and staff. Without this culture change, we will continue to work hard to prevent the common harms but not be prepared to manage the unexpected.
Note :
1- Framework for safe, reliable and effective care. Source: Frankel A, Haradan C, Federico F, Lenocci-Edwards J, et al. A framework for safe, reliable and effective care. White paper. Cambridge, MA: Institute for Heathcare Improvement, 2017. Available from: https://www.ihi.org/resources/Pages/IHIWhitePapers/Framework-Safe-Reliable-Effective-Care.aspx (Cited 12-13-2023).